Are you a night owl or an early bird? Or do you fall in between? I succumbed and bought a wearable device because I thought it could be useful to track my sleep. I spend a few nights in the city every week and I notice that I feel less rested than when I am ‘home’. It seems the right time to buy a wearable device, I am co-organising a Wearables seminar on July 28th 2016 at the Centre for Culture, Ethnicity and Health. I’ve also been invited by Croakey to guest tweet on @WePublicHealth and I want to explore how the concepts of consumer participation, health literacy and cultural competence are changing with technologisation in health care. Check out this interview with Marie McInerney editor at Croakey on Youtube if you are interested in the seminar). I’ve also just started a course at QUT on Social media and data analytics as an entry point into beginning to understand what kinds of data are being generated and what can be done with that.

Jawbone from the Harvey Norman catalogue
Wearable health technologies are growing in social acceptance and use, especially for people interested in fitness and health monitoring as a form of preventative medicine. As sensors become cheaper and smaller, many kinds of health-related data that previously relied upon clinical equipment are becoming available for continuous self-monitoring by patients and consumers. In effect, these technologies are turning the body into media, so that a health consumer can become their own twenty four hour news channel focused entirely on the realtime representation of wellbeing.
Wearable technology platforms have been dominated by the English-speaking middle-classes, (“the wealthy, worried and well” as Michael Paasche-Orlow suggests), limiting the community benefits of enhanced participation and health. Barbara Feder Ostrov notes:
But Fitbits aren’t particularly useful if you’re homeless, and the nutrition app won’t mean much to someone who struggles to pay for groceries. Same for emailing your doctor if you don’t have a doctor or reliable Internet access.
The diffusion of mobile phones (that can also be used as health monitoring devices) indicates that these technologies will only expand to a wider range of users.

What are wearables?
Wearable devices or “wearable technology” and “wearables” refer to electronic technologies or computers that are incorporated into clothing and accessories and worn on the body. They can include smart watches
fitness trackers, head mounted displays, smart clothing and jewellery. They do many things that mobile phones and laptop computers do, but some also have features not seen in mobile and laptop devices. Sensory and scanning features can provide biofeedback and track physiological function. There are also more invasive devices which can implanted such as micro-chips, smart tattoos, pumps.
Why is everyone talking about wearables now?
The world of health information is undergoing significant transformation in the digital era. New media channels such as the Internet allow access to on-demand health information outside of authoritative channels; and new technologies such as fitness trackers and wearables produce a wide range of personal health information. Several trends have increased attention on technologies in health including the democratising role of the internet, leading to the emergence of more intensively informed health consumers who expect more precise and individualised care; the ubiquity and mobility of network communications, allowing the immediate bidirectional transfer of information between individuals and systems; the role of social media in providing networks for sharing both personal data and health experiences; and the increasing cost of health care and the potential for technology to make health management more efficient.
What are the benefits?
Traditionally, much clinical interaction relies on self-reporting by consumers, which is then interpreted by researchers and published for incorporation into practice by health practitioners. Along the way, much important information is “lost in translation”. New consumer healthcare technologies are brokering a shared informational interface between caregivers, clinicians, communities and researchers, allowing practitioners to access richer and more detailed empirical data on health consumer activity and their participation in health-seeking activities. Consumer health technologies offer potential for care to be more equitable and patient-centred. In turn, the impacts of these technologies on health service education, planning and policy are far reaching. More about benefits.
Could wearables enhance independence and participation?
Advances in health mean that residents of industrialized countries live longer, but with multiple, often complex, health conditions. Health technologies can expand the capabilities of the health care system by extending its range into the community, improving diagnostics and monitoring, and maximizing the independence and participation of individuals (Patel, Park, Bonato, Chan and Rodgers, 2012). The United Kingdom’s National Health Service (NHS) is giving millions of patients free health apps & connected health devices in a bid to promote self-management of chronic diseases. Wearable sensors also have diagnostic and monitoring applications, which can sense physiological, biochemical and motion changes. Monitoring could help with the diagnosis and ongoing treatment of people with neurological, cardiovascular and pulmonary diseases including seizures, hypertension, dysrhythmias, and asthma. Home-based motion sensing might assist in falls prevention and help maximize an individual’s independence and community participation.
What are the concerns about wearables?
The technological promise also brings concerns, including the impact on the patient-provider relationship; and the appropriate use and validation of technologies. Technologies are also developed with particular service-users in mind, and rarely designed with the participation of people from structurally and culturally marginalised communities. Despite the ubiquity and access to apps, wearables and websites, the lack of science might preclude behaviour change (e.g. no set of standards) and the “average person” could struggle to choose an app that is effective at changing health behaviour. People are anxious about whether their health data can be used against them. Workplace surveillance and tracking employees has become a health and safety issue. There’s concern about whether we can trust the scientific rigor of the apps we are using, for example the accuracy of the heart rate tracker of the Fitbit and concerns about security.
What impact will technologies have on health professional roles?
Health professionals will have to consider how they work with clients in the context of these technologies. The capacity to review and share healthcare experiences is already available. Technologies will require changes in rules, business models, workflow and roles. The advent of authoritative websites like the Better Health Channel, means that health professionals may no longer be the ultimate gate-keepers of knowledge, their role might shift to being health coaches who empower clients to monitor and improve their health by using their own data. They might have a larger role in care coordination and managing care transitions through the use of mobile health apps. They could play a greater role in research at the point of care through data gathering in research projects. They could play a greater role in evaluating the quality and appropriateness of particular apps. Technology could also free up time to care. Nurses often spend more time collecting information rather than looking after patients. One study showed 60 % of the nurse’s/midwife’s time was spent collecting information and only 15% caring for their patients. ePrescription systems in Sweden, the US and Denmark increased health provider productivity per prescription by over 50%.5. eReferrals in Europe reduced the average time spent on referrals by 97%.6. So, there is potential for the enhancement of health system design: workflow and the coordination of care. There will also need to be better support for innovation as this post from The Medical Startup notes:
How can you innovate where your environment is slow to respond to change, and, despite best intentions, has trouble understanding the few (or many) employees who want to do more, but can’t articulate their feelings? How can you innovate when you risk being penalised or even kicked out of a specialty college that you’ve worked so hard to enter?
Health professionals will also need data management or data analytic skills in order to best use the data wearable health technologies generate. The data will range from public health intelligence (for example tracking outbreaks); using data as a diagnostic tool; to follow up treatment plans; to provide access to the personas, problems, goals and preferences which can then improve the care plan through tailored information and also improve engagement and activation. Health professionals will also need to find ways to prepare patients better for their appointments so that the time they spend is better used.
What kinds of workforce preparation will be necessary for using technologies effectively?
The Digital Skills for Health Professionals Committee of the European Health Parliament surveyed over 200 health professionals about their experience with digital health solutions, and a large majority reported to have received no training, or insufficient training, in digital health technology. The committee recommended continuous education of health professionals in the knowledge, use and application of digital health technology. Curricula will need to be updated to prepare health professionals for using mobile apps/diagnostic and data monitoring tools to the nurses’ repertoire of skills and competencies and larger focus on patient-centered care and consumer engagement in health promotion and maintenance activities. Will there be new roles for ‘informaticians’ whose job is to help download apps, set it up, teach patients how to use it to make health messages more understandable? Educators will need to consider how they teach students to use technology and integrate the use of mobile technology into learning experiences and clinical practice. They’ll need to consider how to use technology such as texts, mobile telephones, or video for health promotion and disease prevention. They will also need an understanding of informatics and how health data are stored, transmitted, and used, as well as the use of the electronic health record in patient-centered care planning (Kennedy, Androwich, Mannone, & Mercier, 2014).
Could benefits be realised for people from CALD backgrounds?
As one of the most culturally diverse communities in the world which accounts for around one-third of migrant settlement in Australia, Victorians born overseas as a percentage of the population have grown by 29 per cent from 2001 to 2011—from just below 1.1 million people to 1.4 million (VARG, 2014). The Auditor General notes in the VARG report (2014) that:
Migrants, particularly those with low English proficiency or poor literacy in their own language, and refugees and asylum seekers are among our most vulnerable members of the community. This is because they often have complex needs, particularly in relation to health, welfare and language services. A whole-of-government approach to the broader area of multicultural affairs should improve integration, reduce duplication and better identify gaps in services.
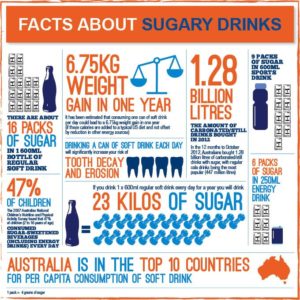
Evidence is growing that the the greater the health literacy of an individual, the greater the likelihood of health maintenance and promotion. Low health literacy is associated with more adverse health outcomes (people with low levels of individual health literacy are between 1.5 and 3 times more likely to experience an adverse health outcome (DeWalt et al. 2004 cited in ACSQHC 2013c). People from refugee and migrant backgrounds may be disadvantaged in the health system because they are in the process of developing their health literacy and capital. Access to and through health care is a significant aspect of feeling a sense of belonging and worth, so improvements in health participation will also have a significant impact on broader social inclusion. We need to explore how low health literacy/data literacy affect the use of health information, merely having access to information in apps is no guarantee that you can use the information.

Last night’s sleep
It’s going to be interesting seeing what data comes out of the Jawbone app. Having had it for two days I can see that it provides useful data about the type of sleep I’ve had. What I do with the information will be one of the questions I grapple with next.
Refs
Health Literacy and Consumer-Facing Technology: Workshop Summary
By Roundtable on Health Literacy, Board on Population Health and Public Health Practice, Institute of Medicine, National Academies of Sciences, Engineering, and Medicine.