Written for and first published in in the August 2016 edition of Nurse Click (the Australian College of Nursing’s monthly electronic, interactive PDF publication available to ACN members, and to stakeholders, the wider nursing and non-nursing community who subscribe to it.). Cite as: DeSouza, R. (2016). Wearable devices and the potential for community health improvement. Nurse Click, August, 14-15 (download pdf 643KB nurseclick_august_2016_final)

TV Glasses (1964)
“Wearable technology“, “wearable devices“, and “wearables” all refer to electronic technologies or computers that are incorporated into items of clothing and accessories which can comfortably be worn on the body. These wearable devices can perform many of the same computing tasks as mobile phones and laptop computers; however, in some cases, wearable technology can outperform these hand-held devices through their integration into bodily movements and functions through inbuilt sensory and scanning features, for example. Wearables include: smart watches, fitness trackers, head mounted displays, smart clothing and jewellery. There are also more invasive varieties including implanted devices such as micro-chips or even smart tattoos, insulin pumps, or for contraception. The purpose of wearable technology is to create constant, seamless and hands-free access to electronics and computers.
Wearables are all about data. Thanks to recent advancements in sensors, we’re able to collect more information about ourselves than ever and use that data to make healthcare personal and tailored to our needs. Traditionally, qualitative health research and much clinical interaction relies on self-reporting by consumers, which is then interpreted by researchers and published for incorporation into practice by health practitioners. Along the way, much important information is “lost in translation”. New consumer healthcare technologies are brokering a shared informational interface between caregivers, clinicians, communities and researchers, allowing practitioners to access richer and more detailed empirical data on health consumer activity and their participation in health-seeking activities.
Consumer health technologies offer potential for care to be more equitable and patient-centred. The technological promise also brings concerns, including the impact on the patient-provider relationship and the appropriate use and validation of technologies. Technologies are also developed with particular service-users in mind, and rarely designed with the participation of people from structurally and culturally marginalised communities. In turn, the impacts of these technologies on health service education, planning and policy are far reaching. It is important that technology is not demographically blind, from a public health and community health perspective it must not reinforce the structural inequalities that exist between those who have access to health and those who haven’t.
The Centre for Culture, Ethnicity and Health, in partnership with the University of Melbourne’s Research Unit in Public Cultures and the Better Health Channel, recently organised a seminar and stakeholder consultation in Melbourne on July 28th with the aim of shaping a research agenda on wearable health technologies and culturally and linguistically diverse (CALD) communities. Typically wearables have been marketed toward the ‘wealthy worried and well’ demographic and the purpose of the seminar was to discuss both the generic issues that emerging wearable technologies present, as well as the unique issues for people from diverse backgrounds. The three hour event brought together clinicians, academics, developers, community organisations, and policymakers to consider the future issues with these technologies.

Seminar. Photo credit Jared Kuvent
The first speaker was University of Melbourne researcher and lecturer Suneel Jethani who expressed scepticism about what wearable health technologies really may deliver for health, particularly for CALD communities. Suneel explored the growth of wearable health technologies through the notion of the pharmakon, the notion that every medicine is also poison, with the devices having capacity to be both beneficial and harmful. Janette Gogler, a Nurse Informatician from Melbourne’s Eastern Health described a randomised control trial of emerging technologies for remote patients with chronic heart failure and chronic obstructive pulmonary disease (COPD). In this trial patients took a number of their own physiological measurements including electrocardiography (ECG) monitoring, blood pressure, and spirometry. While the trial led many patients to feel more in control of their health through a better understanding of their physiology, there were also challenges, including having to manage their expectations of the technology, where patients who became suddenly unwell were upset that the system had not given them forewarning, even though the issues were outside the scope of the devices. Janette also raised the issue of research excluding speakers of additional languages. The final speaker was Deloitte Digital partner Sean McClowry, who noted that the uptake of wearable health technologies has been slower to reach ‘digital disruption’ compared to the smart phones, but saw the likelihood of exponential growth through a new model of care. Sean raised questions about the unprecedented nature of data: how to make it high quality and its analysis meaningful. The session by the three panellists was followed by two youth respondents and a question and answer session and then break out groups which developed further questions and issues for an emerging research program.
In the stakeholder consultation a number of critical themes emerged from many participants: the need to carefully manage privacy; the lack of accuracy of much consumer information; certification of apps; Western models of individual health hard-wired into the platform; the potential of peer support from new technologies; challenges for existing workforces and roles; and the potential of research to stigmatise as well as assist CALD communities. What was agreed was that consumer health technologies were only going to continue to grow and that no part of the health system would be undisrupted by the changes ahead, both intimidating and exciting!
Are you a night owl or an early bird? Or do you fall in between? I succumbed and bought a wearable device because I thought it could be useful to track my sleep. I spend a few nights in the city every week and I notice that I feel less rested than when I am ‘home’. It seems the right time to buy a wearable device, I am co-organising a Wearables seminar on July 28th 2016 at the Centre for Culture, Ethnicity and Health. I’ve also been invited by Croakey to guest tweet on @WePublicHealth and I want to explore how the concepts of consumer participation, health literacy and cultural competence are changing with technologisation in health care. Check out this interview with Marie McInerney editor at Croakey on Youtube if you are interested in the seminar). I’ve also just started a course at QUT on Social media and data analytics as an entry point into beginning to understand what kinds of data are being generated and what can be done with that.

Jawbone from the Harvey Norman catalogue
Wearable health technologies are growing in social acceptance and use, especially for people interested in fitness and health monitoring as a form of preventative medicine. As sensors become cheaper and smaller, many kinds of health-related data that previously relied upon clinical equipment are becoming available for continuous self-monitoring by patients and consumers. In effect, these technologies are turning the body into media, so that a health consumer can become their own twenty four hour news channel focused entirely on the realtime representation of wellbeing.
Wearable technology platforms have been dominated by the English-speaking middle-classes, (“the wealthy, worried and well” as Michael Paasche-Orlow suggests), limiting the community benefits of enhanced participation and health. Barbara Feder Ostrov notes:
But Fitbits aren’t particularly useful if you’re homeless, and the nutrition app won’t mean much to someone who struggles to pay for groceries. Same for emailing your doctor if you don’t have a doctor or reliable Internet access.
The diffusion of mobile phones (that can also be used as health monitoring devices) indicates that these technologies will only expand to a wider range of users.

What are wearables?
Wearable devices or “wearable technology” and “wearables” refer to electronic technologies or computers that are incorporated into clothing and accessories and worn on the body. They can include smart watches
fitness trackers, head mounted displays, smart clothing and jewellery. They do many things that mobile phones and laptop computers do, but some also have features not seen in mobile and laptop devices. Sensory and scanning features can provide biofeedback and track physiological function. There are also more invasive devices which can implanted such as micro-chips, smart tattoos, pumps.
The world of health information is undergoing significant transformation in the digital era. New media channels such as the Internet allow access to on-demand health information outside of authoritative channels; and new technologies such as fitness trackers and wearables produce a wide range of personal health information. Several trends have increased attention on technologies in health including the democratising role of the internet, leading to the emergence of more intensively informed health consumers who expect more precise and individualised care; the ubiquity and mobility of network communications, allowing the immediate bidirectional transfer of information between individuals and systems; the role of social media in providing networks for sharing both personal data and health experiences; and the increasing cost of health care and the potential for technology to make health management more efficient.
Traditionally, much clinical interaction relies on self-reporting by consumers, which is then interpreted by researchers and published for incorporation into practice by health practitioners. Along the way, much important information is “lost in translation”. New consumer healthcare technologies are brokering a shared informational interface between caregivers, clinicians, communities and researchers, allowing practitioners to access richer and more detailed empirical data on health consumer activity and their participation in health-seeking activities. Consumer health technologies offer potential for care to be more equitable and patient-centred. In turn, the impacts of these technologies on health service education, planning and policy are far reaching. More about benefits.
Could wearables enhance independence and participation?
Advances in health mean that residents of industrialized countries live longer, but with multiple, often complex, health conditions. Health technologies can expand the capabilities of the health care system by extending its range into the community, improving diagnostics and monitoring, and maximizing the independence and participation of individuals (Patel, Park, Bonato, Chan and Rodgers, 2012). The United Kingdom’s National Health Service (NHS) is giving millions of patients free health apps & connected health devices in a bid to promote self-management of chronic diseases. Wearable sensors also have diagnostic and monitoring applications, which can sense physiological, biochemical and motion changes. Monitoring could help with the diagnosis and ongoing treatment of people with neurological, cardiovascular and pulmonary diseases including seizures, hypertension, dysrhythmias, and asthma. Home-based motion sensing might assist in falls prevention and help maximize an individual’s independence and community participation.
What are the concerns about wearables?
The technological promise also brings concerns, including the impact on the patient-provider relationship; and the appropriate use and validation of technologies. Technologies are also developed with particular service-users in mind, and rarely designed with the participation of people from structurally and culturally marginalised communities. Despite the ubiquity and access to apps, wearables and websites, the lack of science might preclude behaviour change (e.g. no set of standards) and the “average person” could struggle to choose an app that is effective at changing health behaviour. People are anxious about whether their health data can be used against them. Workplace surveillance and tracking employees has become a health and safety issue. There’s concern about whether we can trust the scientific rigor of the apps we are using, for example the accuracy of the heart rate tracker of the Fitbit and concerns about security.
What impact will technologies have on health professional roles?
Health professionals will have to consider how they work with clients in the context of these technologies. The capacity to review and share healthcare experiences is already available. Technologies will require changes in rules, business models, workflow and roles. The advent of authoritative websites like the Better Health Channel, means that health professionals may no longer be the ultimate gate-keepers of knowledge, their role might shift to being health coaches who empower clients to monitor and improve their health by using their own data. They might have a larger role in care coordination and managing care transitions through the use of mobile health apps. They could play a greater role in research at the point of care through data gathering in research projects. They could play a greater role in evaluating the quality and appropriateness of particular apps. Technology could also free up time to care. Nurses often spend more time collecting information rather than looking after patients. One study showed 60 % of the nurse’s/midwife’s time was spent collecting information and only 15% caring for their patients. ePrescription systems in Sweden, the US and Denmark increased health provider productivity per prescription by over 50%.5. eReferrals in Europe reduced the average time spent on referrals by 97%.6. So, there is potential for the enhancement of health system design: workflow and the coordination of care. There will also need to be better support for innovation as this post from The Medical Startup notes:
How can you innovate where your environment is slow to respond to change, and, despite best intentions, has trouble understanding the few (or many) employees who want to do more, but can’t articulate their feelings? How can you innovate when you risk being penalised or even kicked out of a specialty college that you’ve worked so hard to enter?
Health professionals will also need data management or data analytic skills in order to best use the data wearable health technologies generate. The data will range from public health intelligence (for example tracking outbreaks); using data as a diagnostic tool; to follow up treatment plans; to provide access to the personas, problems, goals and preferences which can then improve the care plan through tailored information and also improve engagement and activation. Health professionals will also need to find ways to prepare patients better for their appointments so that the time they spend is better used.
The Digital Skills for Health Professionals Committee of the European Health Parliament surveyed over 200 health professionals about their experience with digital health solutions, and a large majority reported to have received no training, or insufficient training, in digital health technology. The committee recommended continuous education of health professionals in the knowledge, use and application of digital health technology. Curricula will need to be updated to prepare health professionals for using mobile apps/diagnostic and data monitoring tools to the nurses’ repertoire of skills and competencies and larger focus on patient-centered care and consumer engagement in health promotion and maintenance activities. Will there be new roles for ‘informaticians’ whose job is to help download apps, set it up, teach patients how to use it to make health messages more understandable? Educators will need to consider how they teach students to use technology and integrate the use of mobile technology into learning experiences and clinical practice. They’ll need to consider how to use technology such as texts, mobile telephones, or video for health promotion and disease prevention. They will also need an understanding of informatics and how health data are stored, transmitted, and used, as well as the use of the electronic health record in patient-centered care planning (Kennedy, Androwich, Mannone, & Mercier, 2014).
As one of the most culturally diverse communities in the world which accounts for around one-third of migrant settlement in Australia, Victorians born overseas as a percentage of the population have grown by 29 per cent from 2001 to 2011—from just below 1.1 million people to 1.4 million (VARG, 2014). The Auditor General notes in the VARG report (2014) that:
Migrants, particularly those with low English proficiency or poor literacy in their own language, and refugees and asylum seekers are among our most vulnerable members of the community. This is because they often have complex needs, particularly in relation to health, welfare and language services. A whole-of-government approach to the broader area of multicultural affairs should improve integration, reduce duplication and better identify gaps in services.
Evidence is growing that the the greater the health literacy of an individual, the greater the likelihood of health maintenance and promotion. Low health literacy is associated with more adverse health outcomes (people with low levels of individual health literacy are between 1.5 and 3 times more likely to experience an adverse health outcome (DeWalt et al. 2004 cited in ACSQHC 2013c). People from refugee and migrant backgrounds may be disadvantaged in the health system because they are in the process of developing their health literacy and capital. Access to and through health care is a significant aspect of feeling a sense of belonging and worth, so improvements in health participation will also have a significant impact on broader social inclusion. We need to explore how low health literacy/data literacy affect the use of health information, merely having access to information in apps is no guarantee that you can use the information.

Last night’s sleep
It’s going to be interesting seeing what data comes out of the Jawbone app. Having had it for two days I can see that it provides useful data about the type of sleep I’ve had. What I do with the information will be one of the questions I grapple with next.
Refs
Health Literacy and Consumer-Facing Technology: Workshop Summary
By Roundtable on Health Literacy, Board on Population Health and Public Health Practice, Institute of Medicine, National Academies of Sciences, Engineering, and Medicine.
A winter evening, wet and cold. Squashed into a tram. When a seat became available, I swooped down into it, finding myself next to a woman who proceeded to cover her nose. As she fanned her face with her other hand, I asked her with gentle concern if she was ok. She responded vehemently and with a force I didn’t expect: “It stinks in here, full of people smelling of onions and curry and shit”. Hmm. We were surrounded by Indians including me.

The new super sized E tram leaves the South Melbourne Depot. Pic. Nicole Garmston
It’s not the first time I’ve had funny looks and comments about food and smells but the last time was when it was referring to my lunchbox, quite a few decades ago. The incident on the tram made me think about how smells are political (Manasalan). I’m writing about smells in hospitals in a book chapter coming out later this year and I am interested in what makes some public smells acceptable (for example disinfectant) and other more organic smells not so acceptable or even disgusting.
The food that is a salve for the dislocated, lonely, isolated migrant also sets her apart, making her stand out as visibly, gustatorily or olfactorily different. The soul sustaining resource also marks her as different, a risk. If her food is seen as smelly, distasteful, foreign, violent or abnormal, these characteristics can be transposed to her body and to those bodies that resemble her.

Laksa by Ruth De Souza
Food smells categorise groups of people who are different, and those viewed as negative are seen as a marker of non-western primitiveness. The emotion of disgust is emblematic of the too-near proximity of others and the fear that we might be invaded through our mouths. Probyn writes:
disgust reveals the object in all of its repellent detail, it causes us to step back, and, in that very action, we are also brought within the range of shame
However, nutritional assimilation or sanitisation to become odourless and modern does not guarantee belonging, like citizenship it remains thin when compared to the affective power of ethnic identity. (DeSouza, in press).

Grinding my own spice mix, by Ruth De Souza
I am a committed foodie (defined by Johnston and Baumann, 2010: 61), as ‘somebody with a strong interest in learning about and eating good food who is not directly employed in the food industry’ who is also interested in the politics of food. My partner and I commute to Melbourne, a foodie paradise. Melbourne’s food culture has been made vibrant by the waves of migrants who have put pressure on public institutions, to expand and diversify their gastronomic offerings for a wider range of people. However, our consumption can naturalise and make invisible colonial and racialised relations. Thus the violent histories of invasion and starvation by the first white settlers, the convicts whose theft of food had them sent to Australia and absorbed into the cruel colonial project of poisoning, starving and rationing indigenous people remain hidden from view. So although we might love the food we might not care about the cooks at all as Rhoda Roberts points out:
In Australia, food and culinary delights are always accepted before the differences and backgrounds of the origin of the aroma are.
Sometimes though the acceptance is also class based or related to gentrification take Nick Earles’ point:
But it wasn’t as bad as being the kid from the Italian family who had his “wog” lunch thrown in the bin most days, only to watch the perpetrators spend $10 in cafes 20 years later for the exact same food – focaccia and prosciutto – with no recollection of what they’d done.
It’s been a long time since I’ve experienced someone else’s visible disgust. How to negotiate the smell that is out of place and the identity that does not belong? An ongoing process, but I’ve had plenty of practice.

Jellyfish and cabbage salad, by Ruth De Souza
Unpublished manuscript for those who might be interested. Cite as: DeSouza, R. (2016, July 16). Using forum theatre to facilitate reflection and culturally safe practice in nursing [Web log post]. Retrieved from: http://ruthdesouza.dreamhosters.com/2016/07/16/using-forum-theatre-for-reflective-practice/
High quality communication is central to nursing practice and to nurse education. The quality of interaction between service users/patients and inter-professional teams has a profound impact on perception of quality of care and positive outcomes. Creating spaces where reflective practice is encouraged allows students to be curious, experiment safely, make mistakes and try new ways of doing things. Donald Schon (1987) likens the world of professional practice to terrain made up of high hard ground overlooking a swamp. Applying this metaphor in Nursing, Street (1991) contends that some clinical problems can be resolved through theory and technique (on hard ground), while messy, confusing problems in swampy ground don’t have simple solutions but their resolution is critical to practice.

Rocks Philip Island
Australian society has an Indigenous foundation and is becoming increasingly multicultural.In Victoria 26.2 percent of Victorians and 24.6 per cent of Australians were born overseas, compared with New Zealand (22.4 per cent), Canada (21.3 per cent), United States (13.5 per cent) and The United Kingdom (10.4 per cent). Australia’s multicultural policy allows those who call Australia home the right to practice and share in their cultural traditions and languages within the law and free from discrimination (Australia Government, 2011, p. 5). Yet, research highlights disparities in the provision of health care to Culturally and Linguistically Diverse (CALD) groups and health services are not always able to ensure the delivery of culturally safe practice within their organisations (Johnstone & Kanitsaki, 2008).
An important aspect of cultural safety is the recognition that the health care system has its own culture. In Australia, this culture is premised on a western scientific worldview. Registered nurses (RNs) have a responsibility to provide culturally responsive health care that is high quality, safe, equitable and meets the standards expected of the profession such as taking on a leadership role, being advocates and engaging in lifelong learning. RNs who practice with cultural responsiveness are able to ‘respond to the healthcare issues of diverse communities’ (Victorian Department of Health [DoH], 2009, p. 4), and are respectful of the health beliefs and practices, values, culture and linguistic needs of the individual, populations and communities (DoH, 2009, p. 12).
Culturally competent nursing requires practitioners to provide individualised care and consider their own values and beliefs impact on care provision. Critical reflection can assist nurses to work in the swampy ground of linguistic and cultural diversity. Reflection involves learning from experience: not simply thinking back over an event, but developing a conscious and systematic practice of thinking about experience in order to learn and change future behaviour. Critical reflection involves challenging the nurse’s understanding of themselves, their attitudes and behaviours in order to bring their views of practice and the world closer to the complex reality of care. This kind of process facilitates clinical reasoning, which is the thinking and decision-making toward undertaking the best-judged action, enhancing client care and improve practitioner capability and resilience.
Didactic approaches impart knowledge and provide students with declarative knowledge but don’t always provide the opportunity to practice communication techniques or to explore in depth the attitudes and behaviours that influence their own knowledge. Drama and theatre are increasingly being used to create dynamic simulated learning environments where students can try out different communication techniques in a safe setting where there are multiple ways of communicating. A problem based learning focus allows students to reflect on their own experiences and to arrive at their own solutions, promoting deep learning as students use their own experiences and knowledge to problem solve.
In 2015 I developed and trialed a unit for students at all three Monash School of Nursing and Midwifery campuses in their third year. The aim of the unit was to provide students with resources to understand their own culture, the culture of healthcare and the historical and social issues that contribute to differential health outcomes for particular groups in order to discern how to contribute to providing culturally safe care for all Australians. The unit examined how social determinants of health such as class, gender, race, sexual orientation, gender identity; education, economic status and culture affect health and illness. Students were invited to consider how politics, economics, the social-cultural environment and other contextual factors impacted on Aboriginal and Torres Strait Islander and Culturally and Linguistically Diverse (CALD) communities. Students were asked to consider how policy, the planning, organisation and delivery of health and healthcare shaped health care delivery.
The unit was primarily delivered online but a special workshop was offered using Forum theatre developed by Augusto Boal in partnership with two experienced practitioners Azja Kulpińska and Tania Cañas. Forum theatre is focused on promoting dialogue between actors and audience members, it promotes transformation for social justice in the broader world and differs from traditional theatre which involves monologue. Simulated practices like Forum theatre allow students to address topics from practice within an educational setting, where they can safely develop self-awareness and knowledge to make sense of the difficult personal and professional issues encountered in complex health care environments. This is particularly important when it comes to inter-cultural issues and power relations. Such experiential techniques can help students to gain emotional competence, which in turn assists them to communicate effectively in a range of situations.
Students were invited to identify a professional situation relating to culture and health that was challenging and asked to critically reflect on the event/incident focusing on the concerns they encountered in relation to the care of the person. Through the forum theatre process they were asked to consider alternative understandings of the incident, and critically evaluate the implications of these understandings for how more effective nursing care could have been provided. Through the workshop it was hoped that students could then review the experience in depth and undertake a process of critical reflection in a written assessment by reconstructing the experience beyond the personal. They were encouraged to examine the historical and social factors that structure a situation and to start to theorise the causes and consequences of their actions. They were encouraged to use references such as research, policy documents or theory to support their analysis and identify an overarching issue, or key aspect of the experience that affected it profoundly. Concluding with the key learnings through the reflective process, the main factors affecting the situation, and how the incident/event could have been more culturally safe/competent. Students were asked to develop an action plan to map alternative approaches should this or a similar situation arise in the future.
Forum theatre has been used in nursing and health education to facilitate deeper and more critical reflective thinking, stimulate discussion and exploratory debate among student groups. It is used to facilitate high quality communication skills, critical reflective practice, emotional intelligence and empathy and appeals to a range of learning styles. Being able to engage in interactive workshops allows students to engage in complex issues increasing self-awareness using techniques include physical exercises and improvisations.
My grateful thanks to two Forum Theatre practitioners who led this work with me:
Azja Kulpińska is a community cultural development worker, educator and Theatre of the Oppressed practitioner and has delivered workshops both in Australia and internationally. She has been a supporter of RISE: Refugees, Survivors and Ex-Detainees and for the last 3 years has been co-facilitating a Forum Theatre project – a collaboration between RISE and Melbourne Polytechnic that explores challenging narratives around migration, settlement and systems of oppression. She is also a youth worker facilitating a support group for young queer people in rural areas.
Tania Cañas is a Melbourne-based arts professional with experience in performance, facilitation, cultural development and research. Tania is a PhD candidate at the Centre for Cultural Partnerships, VCA. She also sits on the International PTO Academic Journal.
She has presented at conferences both nationally and internationally, as well as facilitated Theatre of the Oppressed workshops at universities, within prisons and youth groups-in in Australian, Northern Ireland, The Solomon Islands, The United States and most recently South Africa. For the last 2.5 years has been working with RISE and Melbourne Polytechnic to develop a Forum Theatre program with students who are recent migrants, refugees and asylum seekers.
References
- Australian Government. (2011). The People of Australia: Australia’s Multicultural Policy, Retrieved from https://www.dss.gov.au/sites/default/files/documents/12_2013/people-of-australia-multicultural-policy-booklet.pdf
- Boud, D., Keogh, R. and Walker, D. 1985. Reflection: Turning experience into learning. London: Kogan Page.
- Gibbs, G. 1988. Learning by doing: A guide to teaching and learning methods. Oxford: Oxford Further Education Unit.
- Johns, C. 1998b. Illuminating the transformative potential of guided reflection. In Transforming Nursing Through Reflective Practice (eds). C. Johns and D. Freshwater. Oxford: Blackwell Science. 78-90.
- Johnstone, MJ. & Kanitsaki, O. (2008). The politics of resistance to workplace cultural diversity education for health service providers: an Australian study. Race Ethnicity and Education 11(2) 133-134
- McClimens, A., & Scott, R. (2007). Lights, camera, education! The potentials of forum theatre in a learning disability nursing program. Nurse Education Today, 27(3), 203-9. doi:10.1016/j.nedt.2006.04.009
- Middlewick, Y., Kettle, T. J., & Wilson, J. J. (2012). Curtains up! Using forum theatre to rehearse the art of communication in healthcare education. Nurse Education in Practice, 12(3), 139-42. doi:10.1016/j.nepr.2011.10.010
- Nursing and Midwifery Board of Australia (2006). National competency standards for the registered nurse, viewed 16 February 2014: www.nursingmidwiferyboard.gov.au.
- Nursing and Midwifery Board of Australia (2008). Code of professional conduct for nurses in Australia, Nursing and Midwifery Board of Australia, Canberra.
- Schön, D.A. 1987. Educating the Reflective Practitioner. San Francisco: Jossey Bass.
- Street, A. 1990. Nursing Practice: High Hard Ground, Messy Swamps, and the Pathways in Between. Geelong: Deakin University Press.
- Turner, L. (2005). From the local to the global: bioethics and the concept of culture. Journal of Medicine and Philosopy. 30:305-320 DOI: 10.1080/03605310590960193
- Victorian Department of Health. (2009). Cultural responsiveness framework Guidelines for Victorian health services, Retrieved from http://www.health.vic.gov.au/__data/assets/pdf_file/0008/381068/cultural_responsiveness.pdf
- Wasylko, Y., & Stickley, T. (2003). Theatre and pedagogy: Using drama in mental health nurse education. Nurse Education Today, 23(6), 443-448. doi:10.1016/s0260-6917(03)00046-7
- Also see DeSouza, R (2015). Communication central to Nursing Practice. Transforming the Nations Healthcare 2015, Australia’s Healthcare News.
This is a longer version of a foreword in the Winter 2016 edition of the Hive (the Australian College of Nursing’s quarterly publication). After the refs, I’ve added my own experience of living through Cyclone Isaac, which was declared by the Tongan authorities to have been the worst disaster in Tongan history. You can also download the pdf of Receiving the stranger.

#14 Winter 2016, Disaster Health
If one agrees that the manner in which a society receives refugees (the stranger) and upholds their rights is a fairly accurate barometer of the extent to which human rights are generally respected, it follows that an investment in promoting the rights of refugees is a an investment in a more just society for all (Harrell-Bond, 2002, p.80).
This special issue on disaster health acknowledges the relational aspects of being a human. A disaster is the widespread disruption and damage to a community that exceeds its ability to cope and overwhelms its resources (Mayner & Arbon, 2015, p.24). At times of disaster, people need help, and nurses are often on the front line. This is because even outside of what we usually understand to be a disaster, nurses typically work with people and communities who have exhausted their own resources or who need infrastructural and systemic support to galvanise their resources and strength.
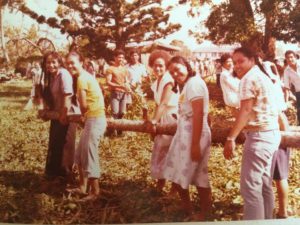
Tonga High School clean up (Photo by Edwin De Souza, 1982).
The call to care that we associate with nursing practice is often juxtaposed with an uncaring social and political context. This leads many nurses to experience moral distress, defined by Jameton (1984) as “aris(ing) when one knows the right thing to do, but institutional constraints make it nearly impossible to pursue the right course of action”. The lack of care in our border discourse reflects how devoid of context the issue of migration is in political debates. Fleeing bodies are objectified and dehumanised by politicians who trumpet xenophobic and alarmist discourses of fear. These discourses are oriented toward a mass media for distribution to people as a proxy for actual engagement with refugees and asylum seekers, underpinning cruel deterrence policies and for-profit detention of vulnerable people. For the practitioner, even if one is concerned, the dominant economic order of neoliberalism keeps us focussed on outputs rather than relationships, we keep our heads down to keep up. Our working situations often pull up the drawbridges to our hearts and selves so we can survive.

Wharf (Photo by Ruth De Souza, 1982).
The work of the three refugee health nurses and an arts practitioner working for refugee support organisation RISE provides important lessons for us, even if we do not work directly with former refugees. The profiles emphasise the relational aspects of nursing: skilled, empathetic, compassionate care that is tailored, solution-oriented, flexible and seen as safe by the recipient. Care which is delivered by providers who are skilled communicators who use interpreters as needed: cultural competence is not about being of a particular culture but of knowing how to bring resources to a new cultural situation where one has limited expertise. The practitioners profiled here continuously attempt to improve through evaluation and overcome resource constraints to work toward models of care that facilitate shared decision-making. And outside the clinical relationship, these practitioners articulate and demand strategic interventions to disrupt institutionalised discourses and practices that have a marginalising effect on vulnerable communities.
Paradoxically, this move from individual to collective and community responsibility – demanding in an individualist culture – can resource our weary hearts, minds and bodies. The critical perspectives foregrounded here draw on new understandings of intersectionality as a key issue in addressing health inequity. They show how categories of difference such as race, gender and class intersect with broader social, economic, historical and political structures to shape experiences of health care. They allow us to look “upstream” (Clark et al, 2015) and to critically evaluate the virulent anti-asylum seeker rhetoric made by politicians and media that refugees and asylum seekers are “trying to take over”, are not “genuine”, are not using the “proper channels”. They surface the often overlooked truth that the Geneva Convention — to which Australia is a signatory — provides people in fear of their lives with a legitimate and legal right to seek asylum. Intersectionality might allow us to engage in cultural safety, to see how our ‘selves’ intersect with the institutional, geopolitical and material aspects of our roles; to consider the investments and conditions that enable us to care and to interrogate the constraints and accountabilities that influence our practice.
Much of the history of critical nursing practice has focused on the “reflective practitioner” (Schön, 1983). However, in the real world there’s rarely time to reflect and institutional demands often preclude reflective time. And reflecting by ourselves assumes we can be fully aware or conscious of ourselves and the social relations that we are a part of. This kind of deliberation cannot adequately address the messy unpredictable nature of nursing contexts.
We might need to start talking to each other again, working in partnership to take part in more socially engaged knowledge practices, where we recognise the limitations of our own knowledge so we are better able to work across difference. Nurses are already skilled at building relationships with clients. We need to extend our therapeutic alliances to families, communities, service providers and community resources. The ACN and nursing’s other professional organisations have taken up the challenge, speaking out against Australian policies and practices that impact on the health outcomes of detainees, asylum seekers and refugees — the secrecy provisions of the Australian Border Force Act of 2015 being a key example. What are our collective responsibilities now? As they have always been: to conduct ourselves with a duty of care. However, in this increasingly complex world, effective care is no longer a matter of caring only for the individual, but requires partnerships that transcend the boundaries of clinical practice, research, education, and political advocacy to work more collaboratively and improve the well being of those marginalised by our nation’s unhealthy policies.
References
Clark, N., Handlovsky, I., & Sinclair, D. (2015). Using Reflexivity to Achieve Transdisciplinarity in Nursing and Social Work (Chapter 9). In L. Greaves, N. Poole, and E. Boyle (Eds.). Transforming Addiction: Gender, Trauma, Transdisciplinarity (pp.120-136). London: Routledge.
Harrell-Bond, B. E (2002). Can Humanitarian Work With Refugees Be Humane? Human Rights Quarterly 24(1):51-85.
Jameton, A. 1984. Nursing Practice: The Ethical Issues. Englewood Cliffs, NJ: Prentice Hall.
Schön, D. A. (1983) The Reflective Practitioner: how professionals think in action London: Temple Smith.
My own experience of disaster: Cyclone Isaac 1982
The Kingdom of Tonga is made up of 170 islands, of which 36 are inhabited. Two-thirds of the population live on Tongatapu the main island. Cyclones occur once every 1.6 years on average.
Cyclone warnings were broadcasted frequently when I went to Tonga High School in 1982. The morning of March 3rd was no different, but this time we didn’t go to school. It was overcast and the wind had picked up. We had a lush tropical garden lovingly tended by my parents with sporadic assistance from their three daughters. The first thing we noticed which was kind of funny, is that it started raining pawpaws, then breadfruit and bananas which I found hilarious. Then it got less funny, banana trees started doubling over, branches started flying past, then sheets of corrugated iron, all the while it was raining hard. We had the sea in front of us and a lagoon behind us, we wondered what it would end. Our electricity supply disappeared and then our neighbours joined us as they were worried about flooding.
Cyclone Isaac was declared by the Tongan authorities to have been the worst disaster in Tongan history, because of the magnitude of the destruction of housing, public buildings and livestock (up to 95% in some
places). According to this shelter case study on disaster mitigation public buildings were designed using seismic and cyclone codes from Australia and New Zealand, but these were not applied to private housing, so some house were built with poorly secured metal roofing sheets (explaining why sheets of corrugated iron had been flying past). What I remember most about that time, was how quickly we all mobilised collectively to clean up the mess and also how quickly international aid arrived.

The front of the house (Photo by Ruth De Souza, 1982).
Cite as: DeSouza, R. (2016, June 1st). Keynote address-Providing Culturally Safe Maternal and Child Healthcare, Multicultural Health Research to Practice Forum: Early Interventions in Maternal and Child Health, Program, Organised by the Multicultural Health Service, South Eastern Sydney, Local Health District, Australia. Retrieved fromhttp://ruthdesouza.dreamhosters.com/2016/06/11/cultural-safety-in-maternity/

Image from the film, the Namesake
A paragraph haunts me in The Namesake, Jhumpa Lahiri’s fictional account of the Indian immigrant experience. Ashoke and Ashima Ganguli migrate from Calcutta to Cambridge, Massachusetts after their arranged wedding. While pregnant, Ashima reflects:
Nothing feels normal. it’s not so much the pain which she knows she will survive. It’s the consequence: motherhood in a foreign land. For it was one thing to be pregnant to suffer the queasy mornings in bed, the sleepless nights, the dull throbbing in her back, the countless visits to the bathroom. Throughout the experience, in spite of her growing discomfort, she’s been astonished by her body’s ability to make life, exactly as her and grandmother and all her great grandmothers had done. That it was happening so far from home, unmonitored and unobserved by those she loved, had made it more miraculous still. But she is terrified to raise a child in a country where she is related to no one, where she knows so little, where life seems so tentative and spare. The Namesake, Jhumpa Lahiri
Ashima’s account beautifully captures the universality of the physical, embodied changes of maternity, the swelling, the nausea and other changes. But what Lahiri poignantly conveys is the singular emotional and cultural upheaval of these changes, the losses they give rise to. The absence of loving, knowledgeable, nurturing witnesses, the absence of a soft place to fall.

Arrival of baby girl in Prato, Tuscany. Credit DeSouza (2006).
In 1994 I worked on a post-natal ward where I was struck by the limits of universality and how treating everybody the same was problematic. For example, ostensibly beneficial practices like the routine administration of an icepack for soothing the perineum postnatally, or the imperative to mobilise quickly or to “room in” have potentially damaging effects on women whose knowledge frameworks differed from the dominant Pakeha culture of healthcare. These practices combined with a system designed for an imagined white middle class user, where professionals had knowledge deficits and monocultural and assimilatory attitudes, led to unsafe practices such as using family members and children as interpreters (my horror when a boy child was asked to ask his mother about the amount of lochia on her pad). The sanctity of birth, requiring the special, nurturing treatment of new mothers and a welcome from a community was superseded by the factory culture of maximum efficiency. Not all mothers were created equal, not young mothers, not older mothers, not single mothers, not substance using mothers, not indigenous mothers, not culturally different mothers. The sense that I was a cog in a big machine that was inattentive to the needs of “other” mothers led me to critique the effectiveness of cultural safety in the curriculum. How was it possible that a powerful indigenous pedagogical tool for addressing health inequity was not evident in clinical practice?

Photo of me as a staff nurse back in the day.
Leaving the post-natal ward, I took up a role helping to develop a new maternal mental health service in Auckland. There too I began to question the limitations of our model of care which privileged talking therapies rather than providing practical help and support. I was also staggered at the time at the raced and classed profile of our clients who were predominantly white middle class career women. Interestingly, the longer I was involved in the service the greater the number of ethnic women accessed the service. For my Master’s thesis, I interviewed Goan women about their maternity experiences in New Zealand, where the importance of social support and rituals in the perinatal period was noted by participants.
As much as it was important to register and legitimate cultural difference, I was also aware of the importance of not falling into the cultural awareness chasm. As Gregory Philips notes in his stunning PhD, it was assumed that through teaching about other cultures, needs would be better understood as “complex, equal and valid” (Philips, 2015). However, it didn’t challenge privilege, class and power. As Joan Scott points out:
There is nothing wrong, on the face of it, with teaching individuals about how to behave decently in relation to others and about how to empathize with each other’s pain. The problem is that difficult analyses of how history and social standing, privilege, and subordination are involved in personal behavior entirely drop out (Scott, 1992, p.9).
The problem with culturalism is that the notion of “learning about” groups of people with a common ethnicity assumes that groups of people are homogenous, unchanging and can be known. Their cultural differences are then viewed as the problem, juxtaposed against an implicit dominant white middle class cultural norm. This became evident in my PhD analysis of interviews with Korean mothers who’d birthed in New Zealand. In Australia and the US, cultural competence has superseded cultural awareness as a mechanism for correcting the limitations of universalism, by drawing attention to organisational and systemic mechanisms that can be measured but as a strategy for individual and interpersonal action, several authors draw attention to competence as being part of the “problem”:
The concept of multicultural competence is flawed… I question the notion that one could become “competent” at the culture of another. I would instead propose a model in which maintaining an awareness of one’s lack of competence is the goal rather than the establishment of competence. With “lack of competence” as the focus, a different view of practicing across cultures emerges. The client is the “expert” and the clinician is in a position of seeking knowledge and trying to understand what life is like for the client. There is no thought of competence—instead one thinks of gaining understanding (always partial) of a phenomenon that is evolving and changing (Dean, 2001, p.624).
In Wellness for all: the possibilities of cultural safety and cultural competence in New Zealand, I advocated for a combination of cultural competence and cultural safety. Cultural safety was developed by Indigenous nurses in Aotearoa New Zealand as a mechanism for considering and equalizing power relationships between client and practitioner. It is an ethical framework for practice derived from postcolonial and critical theory. Cultural safety proposes that practitioners reflect on how their status as culture bearers impacts on care, with care being deemed culturally safe by the consumer or recipient of care. In my PhD I wrote about the inadequacy of the liberal foundations of nursing and midwifery discourses for meeting the health needs of diverse maternal groups. My thesis advocated for the extension of the theory and practice of cultural safety to critique nursing’s Anglo-European knowledge base in order to extend the discipline’s intellectual and political mandate with the aim of providing effective support to diverse groups of mothers. In Australia, cultural responsiveness, cultural security and cultural respect are also used, you can read more about this on my post on Minding the Gap.
So let’s look at culturally safe maternity care. My experience as a clinician and researcher reveal a gap between how birth is viewed. In contemporary settler nations like New Zealand, midwifery discourses position birth as natural and the maternal subject as physically capable of caring for her baby from the moment it is born, requiring minimal intervention and protection. The maternal body is represented as strong and capable for taking on the tasks of motherhood. In contrast, many cultures view birth as a process that makes the body vulnerable, requiring careful surveillance and monitoring and a period of rest and nurturing before the new mother can take on new or additional responsibilities. The maternal body is seen as a body at risk (Mahjouri, 2008), and vulnerable requiring special care through rituals and support. Therefore, practices based on a dominant discourse of birth as a normal physiological event and neoliberal discourses of productive subjectivity create a gap between what migrant women expect in the care they expect from maternal services. These practices also constitute modes of governing which are intended to be empowering and normalizing, but are experienced as disempowering because they don’t take into account other views of birth. Consequently there is no recognition on the part of maternity services that for a short time, there is a temporary role change, where the new mother transitions into a caregiver by being cared for. This social transition where the mother is mothered is sanctioned in order to safeguard the new mother, a demonstration to value and protect both future capacity for mothering and long term well being, in contrast with dominant discourses of responsibilisation and intensive motherhood. Thus, instead of a few days of celebration or a baby shower, extended post-partum practices are enacted which can include the following (Note that these will vary depending on in group differences, urbanisation, working mothers, migration):
- Organised support- where family members (eg mother, mother-in-law, and other female relatives) care for the new mother and infant. Other women may also be involved eg birth attendants.
- Rest period and restricted practices- where women have a prescribed rest periods of between 21 days and five weeks, sometimes called “Doing the month”. Activities including sexual activity, physical and intellectual work are reduced.
- Diet- Special foods are prepared that promote healing/restore health or have a rebalancing function for example because the postpartum period is seen as a time when the body is cold, hot food (protein rich) chicken soup, ginger and seaweed, milk, ghee, nuts, jaggery might be consumed. Special soups and tonics with a cleansing or activating function are consumed eg to help the body expel lochia, to increase breastmilk. These foods might be consumed at different stages of the perinatal period and some food might be prohibited while breastfeeding.
- Hygiene and warmth- particular practices might be adhered to including purification/bathing practices eg warm baths, immersion. Others might include not washing hair.
- Infant care and breastfeeding- Diverse beliefs about colostrum, other members of family may take more responsibility while mother recovers and has a temporarily peripheral role. Breastfeeding instigation and duration may differ.
- Other practices include: binding, infant massage, maternal massage, care of the placenta.
If women are confronted with an unfamiliar health system with little support and understanding, they can experience stress, insecurity, loneliness, isolation, powerlessness, hopelessness. This combined with communication gaps and isolation, poor information provision, different norms, feeling misunderstood and feeling stigmatized. What could be a special time is perceived as a lack of care. Fortunately in Australia there are some excellent resources, for example this research based chapter on Cultural dimensions of pregnancy, birth and post-natal care produced by Victoria Team, Katie Vasey and Lenore Manderson, proposes useful questions for perinatal assessment which I have summarised below:
- Are you comfortable with both male and female health care providers?
- Are there any cultural practices that we need to be aware of in caring for you during your pregnancy, giving birth and postnatal period? – For example, requirements with the placenta, female circumcision or infant feeding method.
- In your culture, do fathers usually attend births? Does your partner want to attend the birth of his child? If not, is there another close family member you would like to be present? Would you like us to speak to them about your care?
- Are there any foods that are appropriate or inappropriate for you according to your religion or customs during pregnancy, birth and the postpartum period?
- Are there any beliefs or customs prohibiting physical activity during pregnancy, birth and the postpartum period? Do you plan to observe these? – For example, a confinement period.
- What is the culturally acceptable way for you to express pain during childbirth? – For example, screaming or trying to keep silent.
- Are there any precautions with infant care?
- How many visitors do you expect while you are in the hospital?
- Do you have anyone in your family or community who can help you in practical ways when you get home?
Negotiating between cultural practices, values and norms, religious beliefs and views, beliefs about perinatal care is a starting point. It is also important to consider language proficiency, health literacy, quality of written materials, and level of acculturation. For further information on health literacy see the Centre for Culture, Ethnicity & Health (CEH) resources including: What is health literacy?, Social determinants of health and health literacy. Using professional interpreters improves communication, clinical outcomes, patient satisfaction and quality of care, and reduces medical testing, errors, costs and risk of hospitalisation. Lack of appropriate interpreter service use is associated with adverse health outcomes. Centre for Culture,Ethnicity & Health (CEH) has excellent resources in this regard: Interpreters: an introduction, Assessing the need for an interpreter, Booking and briefing an interpreter, Communicating via an interpreter, Debriefing with an interpreter, Developing a comprehensive language services response, Language services guide Managing bilingual staff, Planning for translation, Recruiting bilingual staff.
Assessment should also consider:
- Genetics and pregnancy: women’s age, parity, planning and acceptance of pregnancy, pregnancy related health behaviour and perceived health during pregnancy.
- Migration: women’s knowledge of/familiarity with the prenatal care services/system, experiences and expectations with prenatal care use in their country of origin, pregnancy status on arrival in the new industrialized western country.
- Culture: women’s cultural practices, values and norms, acculturation, religious beliefs and views, language proficiency, beliefs about pregnancy and prenatal care.
- Position in the host country: women’s education level, women’s pregnancy-related knowledge, household arrangement, financial resources and income.
- Social network: size and degree of contact with social network, information and support from social network.
- Accessibility: transport, opening hours, booking appointments, direct and indirect discrimination by the prenatal care providers.
- Expertise: prenatal care tailored to patients’ needs and preferences.
- Treatment and communication: communication from prenatal care providers to women, personal treatment of women by prenatal care providers, availability of health promotion/information material, use of alternative means of communication.
- Professionally defined need: referral by general practitioners and other healthcare providers to prenatal care providers
A review by Small, Roth et al., (2014) found that what immigrant and non-immigrant women want from maternity care is similar: safe, high quality, attentive and individualised care, with adequate information and support. Generally immigrant women were less positive about care than non-immigrant women, in part due to communication issues, lack of familiarity with care systems, perceptions of discriminatory care which was not kind or respectful. The challenge for health systems is to address the barriers immigrant women face by improving communication, increasing women’s understanding of care provision and reducing discrimination. Clinical skills including—introspection, self-awareness, respectful questioning, attentive listening, curiosity, interest, and caring.
Also:
- Facilitating trust, control
- Delivering quality, safe care, communicating, being caring, providing choices
- Facilitating access to interpreters and choice of gender of care provider,
- Considering cultural practices, preferences and needs/different expectations for care
- Engendering positive interactions, being empathetic, kind, caring and supportive.
- Taking concerns seriously
- Preserving dignity and privacy
- Seeing a person both as an individual, a family member and a community member
- Developing composure managing verbal and non-verbal expressions of disgust and surprise
- Paradoxical combination of two ideas— being “informed” and “not knowing” simultaneously.
In that sense, our knowledge is always partial and we are always operating from a position of incompletion or lack of competence. Our goal is not so much to achieve competence but to participate in the ongoing processes of seeking understanding and building relationships. This understanding needs to be directed toward ourselves and not just our clients. As we question ourselves we gradually wear away our own resistance and bias. It is not that we need to agree with our clients’ practices and beliefs; we need to understand them and under-stand the contexts and history in which they develop (Dean, 2001, p.628).
Conclusion
In this presentation I have invited you to examine your own values and beliefs about the perinatal period and how they might impact on the care you might provide. I have asked you to consider both the similarities and differences between how women from culturally diverse communities experience maternity and those from the dominant culture. Together, we have scrutinised a range of strategies for enhancing trust, engagement and perinatal outcomes for all women. Drawing on my own clinical practice and research, I have asked you to consider an alternative conceptualisation of the maternal body when caring for some women, that is the maternal body as vulnerable, which requires a period of rest and nurturing. This framing requires a temporary role change for the new mother to transition into being a caregiver, by being cared for, so that her future capacity for mothering and long term well being are enhanced. I have asked you to reflect on how supposedly empowering practices can be experienced as disempowering because they don’t take into account this view of birth. In the context of differing conceptualisations of birth and the maternal body I have drawn special attention to: negotiating between health beliefs; having cultural humility; considering ways in which your own knowledge is always partial; and recommended a range of resources that can be utilised to ensure positive outcomes for women and their families. As health services in Australia grapple with changing societal demographics including cultural diversity, changing consumer demands and expectations; resource constraints; the limitations in traditional health care delivery; greater emphasis on transparency, accountability, evidence- based practice (EBP) and clinical governance (Davidson et al., 2006), questions of how to provide effective universal health care can be enhanced by considering how differing views can be incorporated as they hold potential benefits for all.
Selected references
- Boerleider, A. W., Wiegers, T. A., Manniën, J., Francke, A. L., & Devillé, W. L. (2013). Factors affecting the use of prenatal care by non-western women in industrialized western countries: A systematic review. BMC Pregnancy and Childbirth, 13(1), 8.
- Dennis, C. L., Fung, K., Grigoriadis, S., Robinson, G. E., Romans, S., & Ross, L. (2007). Traditional postpartum practices and rituals: A qualitative systematic review. Women’s Health (London, England), 3(4), 487-502. doi:10.2217/17455057.3.4.487.
- Mander, S., & Miller, Y. D. (2016). Perceived safety, quality and cultural competency of maternity care for culturally and linguistically diverse women in queensland. Journal of Racial and Ethnic Health Disparities, 3(1), 83-98. doi:10.1007/s40615-015-0118.
- Small, R., Roth, C., Raval, M., Shafiei, T., Korfker, D., Heaman, M. Gagnon, A. (2014). Immigrant and non-immigrant womens experiences of maternity care: A systematic and comparative review of studies in five countries. BMC Pregnancy and Childbirth, 14(1).
Additional web resources
- The Victorian Refugee Health Network has maternity resources.
- Opportunities to improve maternal health literacy through antenatal education: an exploratory study, article by Susan Renkert and Don Nutbeam
Unpublished manuscript that never found an appropriate institutional home, but sharing for those who might be interested. Cite as: DeSouza, R., & Butt, D. (2016, June 11). “I had to keep my options open”: White mothers and neoliberal maternity. [Web log post]. Retrieved from: http://ruthdesouza.dreamhosters.com/2016/06/11/i-had-to-keep-my-options-open-white-mothers-and-neoliberal-maternity/
Where patriarchal healthcare institutions saw birth as a process controlled by male doctors and supported by female nurses, contemporary midwifery draws from liberal feminism the concept of “choice” as the marker of maternal agency. However, critiques of neoliberalism locate “informed choice”, “empowerment” and “partnership” as discursive markers of specific capitalist subjectivities that are unevenly distributed among class, race, and sex. The ideology of reproduction as choice aligns with Foucault’s notion of “governmentality”, where the managerial state promotes middle-class discourses of responsibilisation, transformation and empowerment to regulate and maximise the efforts of individuals within the social body. Previous research has shown how maternal care nurses and midwives are instrumental in reproducing these discourses, reflecting white middle-class ideals of the individual service user. This study explored these themes through a secondary discourse analysis on focus groups with white migrant mothers in Aotearoa New Zealand. While migrant mothers noted differences between the New Zealand context and their home nation, unlike ‘other’ migrant mothers they generally adhered to neoliberal requirements to make choices aligned with the expectations of the state. The mothers espoused ideals of natural birth that sat in tension with their notions of informed consumption, reflecting technoscientific discourses that have informationalised the maternal body and interpellated mothers into neoliberal ideologies. The paper argues that attention to the restricted discourses of choice as empowerment illuminates how settler-colonial maternal healthcare systems are limited in their universality, failing to escape cultural and class-based assumptions that empower some mothers at the expense of others. The paper concludes that critical healthcare analysis and methodologies such as cultural safety provide tools for the transformation of these discourses.
Keywords Maternity, whiteness, neoliberalism, Foucault, cultural safety.
Introduction
Midwifery discourses have advanced a feminist vision of women’s empowerment where women usurp patriarchal control of maternity institutions and increase their own power by becoming informed. However, the intrapersonal strategies of information accumulation and behaviour modification can leave structures of power intact and fulfil neoliberal ends. Facilitating a non-authoritarian, woman-centred ethic of care through liberal feminist values (such as individual choice and autonomy) allows mothers to choose to be healthy and productive, while also leading to a reduction in demands on the state as women govern themselves and each other (Collins, 2009). Although midwifery has positioned itself outside dominant norms as an anti-authoritarian discourse, these ‘choices’ are made within a neoliberal consumerist context of health care (Spoel, 2007). Midwifery is simultaneously constructed by these norms and reproduces them, masking new forms of social regulation shaping health care delivery in the process (Skinner, 1999; Spoel, 2006; O’Connell and Downe 2009). Consequently, the emancipatory promise of liberal feminism has disturbingly converged with the economic ‘freedoms’ of neoliberalism, in a discursive formation structured by whiteness. Where previous work established this formation in the discourses of maternal and child health nurses, this paper diagnoses neoliberal discourses employed by white informed consumers.
The dominance of whiteness in Western healthcare systems has been well established (see e.g. Allen, 2006). The liberal theoretical paradigm is deeply embedded in nursing, where those employed in care are rarely able to see how it structures their professional culture, in turn making it difficult to understand how adherence to seemingly neutral and egalitarian values (to white norms) can be oppressive. Whiteness here does not refer only to the visible phenotype of individuals, but to “a cultural disposition and ideology held in place by specific political, social, moral, aesthetic, epistemic, metaphysical, economic, legal, and historical conditions, crafted to preserve white identity and relations of white supremacy” (Bailey & Zita, 2007: vii). Although it is a scientific and cultural fiction like other racial identities, it has a real social impact on the distribution of resources due to a “possessive investment in whiteness” among white individuals (Lipsitz, 2006). A combination of public policy and private prejudice operate simultaneously to create this investment and perpetuate racialised hierarchies that structure access to resources, power and opportunity. Lipsitz contends that white supremacy is less a direct expression of contempt (as usually described by whites who distance themselves from the term), and more a system that protects white privilege and prevents communities of colour from accumulating assets and upward mobility. Complicating any direct identitarianism, Lipsitz contends that non-white people can become agents of white supremacy as well as passive consumers in its hierarchies— not all white people are equally complicit with white supremacy. White dominance and neoliberalism are two powerful and interrelated concepts that describe the systemic and structural forms that produce and reproduce ideal subjectivities. It is this relationship between subjective experience and institutional rationality that this paper seeks to illuminate.
Liberalism and neoliberal maternity
The revalorisation of liberal precepts into the global structures of institutional power termed neoliberalism has been most thoroughly documented by Michel Foucault. Foucault’s analysis of governmentality as “both a political discourse about the nature of rule and a set of practices that facilitate the governing of individuals from a distance” (Larner, 2006: 6) has particular resonance in health and in maternity. The birth of a future citizen is an event with great emotional, biological, cultural and social significance; and consequently the rites and routines that organize birth reflect core cultural values (Fox & Worts, 1999; Reiger, 2008). Maternal and infant public health has been shaped by state concern about the quantity and quality of population in the context of imperial rivalry, both in the centre of empire and the outer edge of white settlement (Lewis, 1988). The “health of the race” and infant health have been a central focus for doctors and politicians, with babies viewed as valuable assets in the struggle for imperial supremacy (Lewis, 1988). While such explicitly racial discourses are today less prevalent, maternity discourses and practices still reflect and reproduce historical and cultural visions of what it is to be a citizen (Georges, 2008). Good mothering and good governing are intimately linked. Foucauldian analysis in health has shown how institutions produce subjects as citizens, where health professionals are not simply individual agents constrained by institutions but develop their values, beliefs and skills within parameters guided (but not fully determined by) those institutions. Healthcare professionals such as nurses and midwives manage key processes through which hegemonic social subjects are reproduced, and thus reflect transformations in ideologies of the public and the citizenry (Fox & Worts, 1999). Maternal health is therefore a rich site to track shifts in public health from a sovereign technique of population management to a global industry in a neoliberal economic system.
Foucault’s analysis in The Birth of Biopolitics identified neoliberalism as the development of a “general regulation of society by the market” (Foucault, 2008: 145). It involves the enforcement of competition (rather than exchange) as the principle of the market in a game which one is not allowed to drop out of, “a sort of inverted social-contract” (Foucault, 2008: 201). Neoliberal economics becomes “no longer the analysis of the historical logic of processes; it is the analysis of the internal rationality, the strategic programming of individuals’ activity” (Foucault, 2008: 222). In this game, economics is redefined as a behavioural science governed by the “relationship between ends and scarce means which have mutually exclusive uses” (Foucault, 2008: 222). This “competitive ratio” is naturalised, and the neoliberal subject “accepts reality” by responding to “systematic modifications artificially introduced into the environment” — becoming “eminently governable” (Foucault, 2008: 270). Through the extension of market values to all institutions and social action, good neoliberal citizens are constructed as choice-making subjects, who take responsibility for maximising their healthy productivity and minimising risks to their health, reducing collective health demands upon the state.
Historically, women’s freedom during pregnancy was constrained by structural or physical factors to ensure the safety of mother and foetus. Improvements in health have led to the emergence of more subtle kinds of governmental regulation, where normalising strategies focussing on individual ‘lifestyle’ have developed in tandem with the new public health and risk discourses (Petersen & Lupton, 1996). Self-regulation through the internalisation of scientific knowledges and medical technologies and the corresponding modification of behaviour have become central to a type of ideal neoliberal subjectivity variously identified as the healthy citizen (Petersen & Lupton, 1996), the active consumer (Fox, Heffernan, & Nicolson, 2009) and the reflexive project of the self (Giddens, 1991).
Mothers are incited to take up the advice and guidance of experts; are incorporated into relations of surveillance and discipline; and are required to monitor and adapt their behaviour against normative discourses. Ideal neoliberal maternal subjects are scientifically literate, meet normative standards, and consume specialty objects and expert advice (Avishai, 2007). They invest in “intensive motherhood”, a pervasive ideology in Western culture that is: “child-centered, expert-guided, emotionally absorbing, labour intensive, financially expensive” Hays (1998: 46).
As Simon and Dippo (1986: 198) note, a historical and material perspective is required to understand the “nonarbitrary specificity” of power relations in the present, “for while the production and reproduction of social forms is a result of what people do, it can never be understood in terms of what they intend.” To that end, contemporary maternal speech must be linked to the historical conditions of its emergence. The history of midwifery development provides structural clues to the emergence of dominant discursive formations of maternity in New Zealand that enable, constrain and contest the narrated experience of migrant mothers.
Midwifery in New Zealand: erosion, erasure and re-emergence
Midwifery’s emergence as an autonomous feminist profession in New Zealand has been shaped by the desire for professional recognition among midwives and feminist aspirations for the control of birth to be returned to women, (Stojanovic, 2008). Midwifery training began in 1904 with the advent of the Midwives Act, prior to which trained midwives were imported from Britain. Free midwifery services became available to all women from 1938, either in their homes or in maternity hospitals (Pairman, 2006). The trends of medicalisation, hospitalisation and nursification eroded the autonomy of midwifery between 1904 and the 1970s (Stojanovic, 2008). For Māori, the Tohunga Suppression Act (General Assembly of New Zealand, 1907) curtailed the active involvement of tohunga (traditional knowledge specialists) in childbirth, and the expertise of Māori birth attendants or tāpuhi remained suppressed as midwives were trained in New Zealand. With fewer tāpuhi assisting birthing women in their homes, childbirth became relocated into state-owned maternity hospitals, which in the colonial view were thought to be safer and cleaner than Māori homes (Simmonds, 2011), even though Māori maternal mortality rose to three times that of non-Māori by the 1960s. Interventions to reduce infant mortality coupled with demands from women for pain-free childbirth increased the medicalisation of birth, leading to doctors supervising midwifery births and holding legal responsibility (Pairman, 2006). Nursification saw the merging of midwifery into nursing, the erasure of the word ‘midwife’ from legislation and the redefinition of the scope of midwifery practice within nursing (Stojanovic, 2008).
Autonomous midwifery practice (differentiated in scope from nursing) re-emerged through mutually beneficial political lobbying by consumers and midwives forcing legislative changes in the late 1980s. Spurred by decades of feminist struggle, maternity consumer activists saw autonomous midwifery practice as a mechanism for gaining increased control over their own birthing (Pairman, 2006). This pressure eventually led to the passing of the Nurses Amendment Act in 1990 which provided New Zealand women with the option of a caregiver (Lead Maternity Carer or LMC) who could either co-ordinate or provide the care they required from early pregnancy to six weeks postpartum (Pairman, 2006). Consequently, 75.3% of New Zealand women were registered with a midwife to provide lead maternity care in 2007 (Ministry of Health, 2007). Hence, partnership with women became a central tenet of New Zealand midwifery and to its claim as protector of the health of women from an intervening medical corpus (Reiger, 2008). The discourse of ‘partnership’ positions women as ‘naturally’ equipped and capable of carrying and delivering babies without physician monitoring or intervention in hospitals (Macdonald, 2006). The social model of this discourse locates risk not within the female body as under the medical model, but from power relations in the social world including poor support for women. In response, midwives have the capacity to nurture and empower the autonomous woman so that she is capable of birth without intervention (Lane, 2012). The study discussed here consisted of focus groups with mothers and maternal care professionals to evaluate the effects of these discourses and institutional arrangements on different groups of migrant women.
Study Design
The focus groups for this project were undertaken with the assistance of The Royal New Zealand Plunket Society (Plunket), and consisted of focus groups with five ethno-cultural groupings of new migrant mothers (including white mothers) about their maternity experiences (DeSouza, 2006; DeSouza, 2011). Ten first time mothers aged between 29-40 years, who had been living in New Zealand for between two and ten years took part in the white focus group. The women self-identified as ‘white’ and had migrated from South Africa (Jane and Charlotte), England (Nancy, Annette, Olive, Sarah, Carol), the US (Joan and Mary) and Scotland (Georgina). Four had post-graduate qualifications; four had under-graduate qualifications and one a trade certificate. Their occupations included: teacher, scientist, project manager, account manager, project manager, lecturer. Reasons for migrating included the New Zealand lifestyle and their husband’s careers. The group are not intended to be representative of all white female migrants, although the demographic bias of white migrants to New Zealand skews toward the upper-middle class. Of interest here are the range of available subject positions in the discourses represented and what implications those subject positions hold. Discourse analysis can aid understanding of the relationship between “subjectification (the condition of being a subject) and subjectivity (the lived experience of being a subject)” (Walkerdine, 2001: 20). In this case, the focus is on discourses of knowledgeable consumption, natural birth, and intensive motherhood.
Knowledgeable antenatal consumers
Mary invokes liberal feminist/woman centred tenets of choice, freedom and autonomy when she speaks about becoming pregnant through assisted reproductive technologies:
Mary: Artificial insemination… was something that was incredibly easy in New Zealand whereas in the States it would’ve been a lot more difficult and more expensive. For us moving to New Zealand was partly a life-style choice, we had a known donor and we found that we went to a fertility class and it was just incredible how helpful and inclusive they are and everything was really easy to do… more information is always good for us and we found that there was plenty of information for us. It’s like I said before we’ve been planning this for over five years so that was, their resources were there for us.
Mary’s excerpt reflects the liberal feminist ideal of a planned pregnancy and the control of reproductive processes (even in the context of assisted fertility), to which the democratisation of knowledge, its acquisition and demystification are fundamental. Mary positions herself as a responsible health consumer who makes choices (including migrating), within a caring and available system. She actively searches for and chooses the appropriate information, products and services from a saturated global market. Migration is a space where she can realise possibilities for mobility and self-actualisation, imbricating maternity in local and global patterns of consumption. Annette also positions herself as a knowledgeable and responsible consumer, who can both evaluate and challenge expert knowledges:
Annette: Although our doctor suggested certain paths that we could take I wasn’t necessarily in total agreement with what he wanted so I was trying to combine his knowledge with the information that I was reading as well.
Annette’s capacity to act and make choices is evident in her avoidance of informal and embodied knowledge in favour of formal knowledge:
Annette: When I found that I was pregnant the first thing I did was I bought a book named New Zealand Pregnancy Guide… although we have a lot of friends here I didn’t feel that I was in a position where I wanted to talk to anybody about the pregnancy because it was so early and I felt that the more people that I talked to and asked for their advice then if I did miscarry I’d have to tell everybody that I’d miscarried. So I was in that situation of having to try and discover a lot of information out by myself initially and I found that was a little bit overwhelming at times. But that book was particularly useful and then I phoned I think the Ministry of Health and got a list of midwives. And then to be quite honest it was absolutely useless, because I just looked at this list and I’m going, ‘well where do I start’? So you are in this catch 22 thinking ‘do I phone this person? Would they come to me because we’re on the other side of town?’ I didn’t have any recommendations. It was literally a list and it meant nothing to me.
Annette’s preference for purchasing a book of expert knowledge about pregnancy in New Zealand—rather than seeing her networks and friends as primary resources—is emblematic of her desire to produce herself as an autonomous, composed, and rational individual, avoiding public judgement upon her possible failure to reproduce. Her unwillingness to expose her pregnancy and potentially complicate social relationships means that she loses out on possible social support, information and referrals, which could enable the transition to parenthood.
Natural birth
The rewards of antenatal preparation are realised when women describe feeling informed and in control of their birth experiences, aligning with midwifery discourses of natural birth (Brubaker & Dillaway, 2009).
Mary: Well I thought we were going to have a very sort of natural birth with no drugs although I was hoping to take drugs if I was in pain. I found the antenatal explanation of how what happens in a C-section very useful as I ended up having a C-section. And the fact that they explained, ‘ok all of these people are going to be there and it’s going to be a person on your right is going to be your doctor and the person with the baby’, and all of that… I had a really negative reaction to all the drugs and when she explained again who was going to be in the room it was exactly the same as what the antenatal person had said.
Mary’s antenatal preparation equips her for an unintended Caesarean, but instead of feeling cheated by the requirement for medical intervention, she surfaces the woman-centred natural birth discourse of feeling in control and informed. Thus birth can be considered ‘natural’ despite medical intervention, as long as the labouring mother chose the intervention (Macdonald, 2006).
Charlotte’s narrative also captures the two competing discourses of birth that Mary situates herself in. On the one hand, Charlotte values having self-control (through being informed and behaving accordingly) and on the other is willing to surrender control—the choice to rescind action is also a choice (Lupton, 1994):
Charlotte: I just have to say to myself you know we’ve even had to go with the flow, and then also those booklets that you receive on feeding, those pamphlets. I did a lot of reading and my midwife gave me a lot of information. The information from those pamphlets helped me a lot and so I felt comfortable, like I’m on the right track now so everything is going well. So I was trying to speak to myself and keep calm (speaks quietly). I was in labour for since the Saturday and I gave birth on Monday morning so (laughter) I had to keep my options open as well about taking drugs so you know things like that.
Charlotte presents herself as a self-efficacious middle class maternal subject, able to internalise information and adapt her behaviour accordingly through self-discipline, self-denial and will power. Disciplining herself by subsuming her own distress and fear, aligns with the needs of the institution for calm consumers, who are more compliant and require less time and support than distraught ones.
Being given the right information at the right time made Charlotte feel supported:
Charlotte: The midwife that delivered my baby is actually from New Zealand but she worked in Cape Town for three years so that was good, that connection. She told me, step by step where and what stage I’m at. I think that’s the biggest support that you really need in the delivery room is to tell you at what stage you are at and what’s happening.
It is significant that Charlotte constructs her midwife as the person who delivers her baby rather than facilitates Charlotte’s ability to birth her baby. She discursively positions her midwife as a translator, who can link what is happening in her body to an identified physiological process. This positioning challenges midwifery discourses of the mother as ‘expert’ as the midwife’s role as a translator reinforces a hierarchy reminiscent of biomedicine.
Jane actively and discursively resists biomedical discourses, until she acquiesces to Entonox:
Jane: I was trying to still keep my energy up by eating and drinking as much water as possible. My choice was that I wanted to stay at home as long as possible, I didn’t want to be in the hospital for too long because when I start thinking of all the other options, and I wanted a natural childbirth, no assistant and also no pain relief. At the end for about 2 ½ hours before baby was delivered I chose Entonox with the gas and that helped. As the pamphlets also say I actually felt distance from the actual experience so if I think back I would’ve actually chosen nothing but I just felt at that stage I needed something and I chose that. So fortunately baby was in the right position, in a good position so I didn’t have to have a Caesarean. I was more scared of the Caesarean than the pain and I wanted a natural childbirth.
Jane positions herself within midwifery discourses of natural birth, disciplining her body so that she avoids hospital as much as she can, and engaging in deliberate bodily maintenance so she can maximise the efficiency of her body and have the energy to labour. She constructs a natural birth as one where she uses pain relief as a last resort.
Nancy disciplines her body through specific breathing techniques learned outside the health system:
Nancy: Yes. At the beginning of my pregnancy I was kind of really worried about actually giving birth. But what really helped me was I went to do yoga in pregnancy and through that they talked a lot about it and they did sort of breathing and just general exercises to help you kind of keep calm and focused. And at the end of it I really wasn’t worried about it at all and I thought I might even be able to get through this without drugs but I didn’t in the end, I gave in, in the last couple of hours.
Nancy positions herself as a good mother to be, taking control and acting to promote her own health and wellbeing through natural breathing. Nancy’s expectation that her body would be able to cope with birth naturally and without medical intervention reflects her incorporation in woman centred/natural birth discourses. Her acceptance of a biomedical intervention in the form of pain relief in the last few hours is presented as a capitulation, and reflects her perception of the control she had in the process and her failure to accomplish a natural process.
Intensive motherhood
The post-partum period is characterised by the demands of intensive mothering. Producing oneself in the discourses of the “good mother” requires taking sole responsibility for the well-being of the infant while being isolated and having minimal support. The post-natal ward represents a space where the rude transition from women-centred discourses to intensive mothering begins. There is a glaring shift from one-to-one attention from midwives, to competition for support and assistance with other new mothers:
Olive: I mean the actual labour and delivering – fantastic. I couldn’t fault them and the staff was superb, the midwife was just brilliant, the obstetrician fantastic. When I got on the ward I found it really hot, I felt really overwhelmed. I was right next to this buzzer and it just went buzzing all the time because everybody wanted help, I found that really quite distressing and I was absolutely knackered.
The clamour of the buzzer and interruptions signal a consequence of being returned to the factory model of maternity. Olive experiences a shift from care described in superlative terms to feeling overwhelmed, distressed and tired. Meanwhile, Nancy recognises that her expectations were primarily oriented to the birth event with no real preparation for the post-partum period:
Nancy: I just want to say in terms of thinking after the birth, and how it was compared to expectations, I didn’t really have any expectations of after the birth, everything was concentrated about the labour and, ‘oh God, it’s going to feel terrible’ and after the birth it just hit me like that and it was hell for six weeks more or less it was just hell… Yes and I wished somebody had actually told me that it was going to be that hard.
Nancy assumes that if she had been given the information, this post-partum period would have been easier for her, reflecting the notion of autonomous rational personhood that with planning and control of one’s circumstances, future success can be ensured (Wall, 2010).
Interviewer: What was the “hell”?
Nancy: Mainly lack of sleep, lack of sleep and just coping with a crying baby, and I had my Mum and I was lucky she was there for the first three weeks and she did the housework, the cooking and stuff. [Group laughter]
Jane: I also think you also just feel like a robot, cleaning the bottles, making a bottle, breast-feeding, in a little corner all the time, just you and the baby.
The mothers in the group identify a conspiracy of sorts. Much of their preparation for the world of parenthood revolved around knowledge acquisition, maintaining good health during their pregnancies and having control during their labour, none of which help in the postnatal period.
In the quotes that follow, the limitations of expert knowledge and self-sufficiency are identified and Nancy identifies the difference support might make for her.
Nancy: It would’ve been different in that I would’ve had a lot more support and for me a lot of my anxieties around that was I didn’t have anyone to talk to, and particularly (baby crying). And yes OK you meet people at your antenatal group but at that time they’re not your closest friends that you can say anything too. And having said that I did, you know… But I think that was it for me was thinking, ‘oh my God, I just need some adult conversation’. And that’s what I struggled with most probably.
Emotional support and having a confidant require time and energy, and an investment, which can be drawn on. The friendships Nancy has made cannot be drawn on for the kind of support she needs. For Georgina, the absence is emotional as well as practical—in the form of having ‘time out’ for errands or for ‘couple time’:
Georgina: Yes you do miss the support network, friends as well. I’ve got a lot of friends back home who have got kids and I think you miss that as well… Not just family but friends who would maybe be a bit more candour than you might take from them or what you feel than you take from close family and things. So I definitely miss that and also, we were just back home and it was just so nice…you know tight as you are, what simple things, like I needed to go out and do couple of things and I knew I was only going to be half an hour or so and to actually have somewhere to leave him and it would take me half the time.
Discussion and Conclusion
Women who identified as ‘white’ in this study constructed themselves within liberal feminist and neoliberal discourses as consumers who were rational unified actors. They were interpellated as competent selectors and consumers of maternity services, and moral value was attached to their ability to engage in self-reliant behaviours. They embraced the neoliberal psychological imperative to improve and transformed themselves, responding positively even in the most difficult of situations (Baker, 2009). These practices reflect women’s engagement in ‘techniques of the self’ that are constitutive of neoliberal subjectivity. The white mothers conform to the ideal of the good mother (to be) by discursively positioning themselves as taking appropriate individual care and responsibility for their pregnancies and maternal care.
The speech of the women reflects three specific discourses of liberal feminist maternity that form the basis of normative midwifery ideologies.
Firstly, the women routinely position themselves as knowledgeable consumers of authoritative maternity information provided by the health system. Critically interrogating the authority of biomedicine by coordinating and evaluating diverse sources of information is central to woman-centred discourses, where acquiring authoritative knowledge both bypasses medical control and is a way to claim empowerment, subjectivity and agency (Edwards, Davies, & Edwards, 2009). Her ‘preparation’ for motherhood through the acquisition of knowledge valorises scientific/professional knowledge rather than the informal and personalised information or social and emotional support that friends and extended family can provide (Marshall & Woollett, 2000). Authoritative professionals transmit information to individual women whose embodied, enculturated understandings and experiences are discounted or devalued. Yet individual women are expected to engage in reflexive techniques and /or practices of subjectification, to be accountable for the choices that are made, and to account for their behaviours to those who are tasked with monitoring and validated for monitoring them (Stapleton & Keenan, 2009). Thus regulatory technologies “construct an autonomous subject whose choices and desires are aligned with the objectives of the state and other social authorities and institutions” (Petersen & Lupton, 1996: 64).
Secondly, natural birth is positioned as a goal, suppressing technical and industrial discourses associated with medicalisation, except as far as they are in control of the mother. The women articulate being informed and having control, autonomy or authority despite experiencing various degrees of obstetric intervention. As middle-class women are more likely to receive the birth and/or medical treatments they desire, pregnancy and childbirth can be framed as contributing to their personal growth (Brubaker, 2007). In this paradigm of actualisation, it is assumed that intentional actions, self-discipline, self-denial and will power will achieve the ‘right’ kind of birth, and that intervention from a public health system is not a default practice but a considered choice of the mother based on information. In other words, a ‘natural birth’ does not happen naturally, but is chosen as an expression of the knowledgeable consumption discussed above.
Finally, the excerpts on intensive motherhood highlight how this responsibility for maternal self-expression and knowledge is a critical instrument of women’s control in the post-partum period. The mother’s needs are marginalised, as mothers take on most of the responsibility for nurturing and developing the sacred child. Pregnant women and their partners are subject to discipline, given that they are held responsible for maximising their own health and that of their foetus‘ and then infant’s body (Collins, 2009). Intensive mothering is intertwined with a neoliberal rationality, where individual responsibility and self-management are fore-grounded and social support is reduced compared with earlier in the perinatal period (Wall, 2001). Neoliberal discourses place individual responsibility for parenting on mothers, shifting the costs and the burden of work from public resources to household resources. The gendered aspects of these discourses are visible in the assumptions of reproductive heteronormativity, where market production separates the private and public spheres with women taking responsibility for childrearing. These discourses assume that households are based on a nuclear family; that caring labour is divided on the basis of gender, and that this labour is elastic and must expand to fit demand. In turn, the domain of the private is subject to surveillance and regulation to account for responsibilisation, or the ways in which public tasks become the responsibility of individuals, the private sector and community (Schinkel & Van Houdt, 2010; Clarke, 2004). In the postpartum, women note that they are treated like a “normal person”, a labouring, productive figure rather than the choice-making perinatal consumer. The responsibilities for infant care and repetitive ‘robotic’ household tasks seem overwhelming, and there is a sense of failure and disillusionment with the system and with providers that cannot be displaced through their well-developed information gathering strategies.
The interplay of the three discourses has significant implications for maternal mental health, as they locate the “specialness” of birth in decisions which are seen to be under the mother’s individual control, when in fact broader class positions are strongly determinant of what services and support are available. The incentives to locate maternal knowledge in an individual relationship with an authoritative caregiver produce dependence on a system that shifts risk and responsiblity onto the individual. These assumptions come to structure the professional habitus of nursing and midwifery professionals, who adopt regulatory behaviours that fail to support women who do not subscribe to white middle-class ideals. Governing occurs through the aspirations of mothers, and while the state appears to be protecting the interests of infants and parents, little in the way of actual resources are provided. These neoliberal discourses of individual responsibility constructed through dependence on knowledge also disempower women who do subscribe to these ideals, as the institutional withdrawal of support in postnatal care cannot be addressed by the skills the knowledgeable consumer has developed.
Conclusion
In recent decades the capacity of liberal feminist frameworks to provide effective support to non-Western women has been questioned, and midwifery has not been exempt. In New Zealand, the discursive emphasis of being ‘with woman’ implied in the etymology of the word midwife is central to indigenous critiques of Pākeha (white/European) midwifery (Kenney, 2011). Kenney notes that the Pākeha liberal feminist agenda privileges the individual while neglecting the familial context of pregnancy and birth. In contrast, the Māori word for midwife ‘kaiwhakawhānau’ emphasises the facilitation, creation and development of whānau (family). This discursive contrast between Māori models of midwifery has heightened significance in the context of the under-representation of Māori midwives (6.4%) when Māori births comprise approximately 28% of total births and in the context of and inequalities in birth outcomes between Māori and non-Māori (New Zealand Health Information Service 2010 cited in Kenney 2011; Ratima& Crengle, 2012). Midwifery as a profession has attempted to redress these injustices by incorporating Māori cultural principles and values (Ngā Turanga Kaupapa) in midwifery practice competencies (Kenney, 2011), and the development of cultural safety has become a central, if contested tenet of nursing education in New Zealand (Ramsden 1997; DeSouza 2008).
A consistent aim of cultural safety training in nursing has been to deconstruct the implicit racism of the healthcare system, by asking practitioners to reflect on one’s practice, values and cultural assumptions (Browne et al., 2009). In other words, it asks all of us involved in the health system to understand our own position as culture-bearers. Yet, the assumptions of white culture are hard to identify as the norms and commitments of whiteness are naturalised by their ubiquity and dominance. This culture not only shapes practitioner values but also shapes the dominant voices of those consumers who receive and evaluate care, while marginalising women outside these cultural assumptions. Operationalising critical feminist and postcolonial critiques through cultural safety can help nurses understand how the discourses they use are shaped by wider social discourses, which can then be critically interrogated (Browne, 2005). This analysis has aimed to contribute to this project by identifying three norms of white maternity that are normalised in alignment with neoliberal principles: the knowledgeable consumer, natural birth and intensive motherhood. These norms contrast to the discourses that have been identified in the literature on migrant maternity, which generally reflect less of an individualised focus on choosing the experience of birth and more on the presence or exclusion of wider family and social supports. Given the shock and isolation many women experience in the transition from impending mother to intensive mothering, critically advocating for those diverse structures of support can potentially benefit all mothers.
References
Allen DG (2006) Whiteness and difference in nursing. Nursing Philosophy 7(2): 65–78.
Avishai O (2007) Managing the lactating body: The breast-feeding project and privileged motherhood. Qualitative Sociology 30(2): 135-152.
Baker J (2009) Young mothers in late modernity: Sacrifice, respectability and the transformative neo-liberal subject. Journal of Youth Studies 12(3): 275–288.
Browne AJ (2005) Discourses influencing nurses’ perceptions of First Nations patients. Canadian Journal of Nursing Research 37(4): 62–87.
Browne AJ, Varcoe C, Smye V, Reimer-Kirkham S, Lynam M, and Wong S (2009) Cultural safety and the challenges of translating critically oriented knowledge in practice. Nursing Philosophy 10(3): 167–179.
Brubaker SJ and Dillaway HE (2009) Medicalization, natural childbirth and birthing experiences. Sociology Compass 3(1): 31–48.
Clarke J (2004) Dissolving the public realm?: The logics and limits of neo-liberalism. Journal of Social Policy 33(1): 27–48.
Collins EA (2009) Governing partners: responsibilization in pregnancy advice literature for men. Unpublished doctoral thesis. Victoria: University of Victoria.
DeSouza R (2006) New spaces and possibilities: The adjustment to parenthood for new migrant mothers. Wellington: Families Commission.
DeSouza R (2008) Wellness for all: the possibilities of cultural safety and cultural competence in New Zealand. Journal of Research in Nursing 13(2): 125–135.
DeSouza R (2013) Regulating migrant maternity: Nursing and midwifery’s emancipatory aims and assimilatory practices. Nursing Inquiry 20(4): 293-304.
Edwards M, Davies M and Edwards A (2009) What are the external influences on information exchange and shared decision-making in healthcare consultations: A meta-synthesis of the literature. Patient Education and Counseling 75(1): 37–52.
Foucault M (2008) The Birth of Biopolitics: Lectures at the Collège de France 1978-1979. Basingstoke: Palgrave Macmillan.
Fox B and Worts D (1999) Revisiting the critique of medicalized childbirth: A contribution to the sociology of birth. Gender and Society 13: 326-346.
Fox R, Heffernan K and Nicolson P (2009) “I don’t think it was such an issue back then”: Changing experiences of pregnancy across two generations of women in South-East England. Gender, Place & Culture 16(5): 553–568.
Frankenberg R (1993) White women, race matters: The social construction of whiteness. Minneapolis: University of Minnesota Press.
Freda MC (2001) If given the choice. MCN: The American Journal of Maternal/Child Nursing 26(3): 117.
General Assembly of New Zealand (1907) An Act to suppress Tohunga. Statute No: 13. Wellington: Government Print.
Georges E (2008) Bodies of knowledge: The medicalization of reproduction in Greece. Nashville: Vanderbilt University Press.
Giddens A (1991) Modernity and self-identity: Self and society in the late modern age. Stanford: Stanford University Press.
Harvey D (2005) A brief history of neoliberalism. Oxford: Oxford University Press.
Hays S (1998) The cultural contradictions of motherhood. New Haven: Yale University Press.
Hunn JK (1961) Report on the Department of Maori Affairs, with Statistical Supplement, 24 August 1960. Appendices to the Journal of the House of Representatives, G.10. Government Printer, Wellington.
Kenney C (2011) Midwives, women and their families: a Maori gaze. Towards partnerships for maternity care in Aotearoa New Zealand. AlterNative: An International Journal of Indigenous Peoples 7(2).
Lane DK (2012) Dreaming the impossible dream: ordering risks in Australian maternity care policies. Health Sociology Review 21(1): 23–35.
Larner W (2006) Brokering citizenship claims: Neo-liberalism, biculturalism and multiculturalism in Aotearoa. In: E Tastsoglou and AZ Dobrowolsky (eds) Women, migration, and citizenship: Making local, national, and transnational connections. Hampshire: Ashgate, pp. 131–148.
Lewis M (1988) The ‘health of the race’ and infant health in New South Wales: Perspectives on medicine and empire. In: RM MacLeod and MJ Lewis (eds) Disease, medicine, and empire: perspectives on Western medicine and the experience of European expansion. London: Routledge, pp. 301–315.
Lupton D (1994) Medicine as culture: Illness, disease and the body in western societies. London: Sage.
Macdonald M (2006) Gender expectations: Natural bodies and natural births in the new midwifery in Canada. Medical Anthropology Quarterly 20(2): 235–256.
Marshall H and Woollett A (2000) Fit to reproduce? The regulative role of pregnancy texts. Feminism and Psychology 10(3): 351–367.
Ministry of Health (2007) Notice Pursuant to Section 88 of the New Zealand Public Health and Disability Act 2000. Wellington: Ministry of Health.
Mookherjee M (2005) Affective citizenship: Feminism, postcolonialism and the politics of recognition. Critical Review of International Social and Political Philosophy 8(1): 31–50.
Nairn RGR (2003) Madness, media & mental illness: A social constructionist approach. Unpublished doctoral thesis. Auckland: University of Auckland.
O’Connell R and Downe S (2009) A metasynthesis of midwives’ experience of hospital practice in publicly funded settings: compliance, resistance and authenticity. Health (London) 13(6): 589—609.
Pairman S (2006) Midwifery partnership: Working with women. In: L Page and R McCandlish (eds) The new midwifery: Science and sensitivity in practice (2nd ed.). Philadelphia: Elsevier/Churchill Livingstone, pp. 73–97.
Petersen AR and Lupton, D (1996) The new public health: Health and self in the age of risk. St Leonards, NSW: Allen & Unwin.
Powers P (2001) The methodology of discourse analysis. Mississauga, Ontario: Jones & Bartlett Publishers.
Ratima M and Crengle S (2012) Antenatal, labour, and delivery care for Maori: Experiences, location within a lifecourse approach, and knowledge gaps. Pimatisiwin: A Journal of Aboriginal & Indigenous Community Health 10(3): 353–366.
Reiger K (2008) Domination or mutual recognition? Professional subjectivity in Midwifery and Obstetrics. Social Theory & Health 6(2): 132–147.
Schinkel W and Van Houdt F (2010) The double helix of cultural assimilationism and neoliberalism: Citizenship in contemporary governmentality. The British Journal of Sociology 61(4): 696–715.
Simmonds N (2011) Mana wahine: Decolonising politics. Womens Studies Journal 25(2): 11–25.
Simon RI and Dippo D (1986) On Critical Ethnography Work. Anthropology & Education Quarterly 17: 195–202.
Skinner J (1999) Midwifery partnership: individualism contractualism or feminist praxis? New Zealand College of Midwives Journal 21: 14–17.
Spoel P (2007) A feminist rhetorical perspective on informed choice in midwifery. Rhetor: Journal of the Canadian Society for the Study of Rhetoric 2: 1–25.
Stapleton H and Keenan J (2009) Bodies in the making: Reflections on women’s consumption practices in pregnancy. In: F Dykes and VH Moran (eds) Infant and young child feeding: Challenges to implementing a global strategy. Ames, Iowa: Blackwell, pp. 119–127.
Stojanovic J (2008) Midwifery in New Zealand 1904-1971. Contemporary Nurse 30(2): 156–167.
Wall G (2001) Moral constructions of motherhood in breastfeeding discourses. Gender and society 15(4): 592–610.
Acknowledgements
Many thanks to Debbie Payne, David Allen, Ray Nairn and Tim McCreanor for their helpful conversations and feedback.

